Health insurance policies are often filled with jargon, which can make it difficult for policyholders to fully benefit from comprehensive health coverage.
Companies like ACKO Insurance provide easy-to-understand coverages and benefits. To make health insurance more user-friendly for everyone, the IRDAI has launched new regulations. Let's understand the key changes and how they can impact your policy and coverage.
#1 Moratorium period
The moratorium period is the period after which the insurers can reject health insurance claims only because of fraud or other permanent exclusions. Previously, this moratorium period was eight years, which has recently been reduced to five. This means that policyholders' claims cannot be rejected for misrepresentation of information after 60 months of continued coverage (including migration and portability).
#2 Pre-Existing Diseases (PED)
Insurers often fail to cover PEDs, at least until the waiting period, but there is a lack of clarity on what can be declared as PEDs. Effective April 1, 2024, a PED is any ailment, condition, disease, or injury diagnosed or treated or medical advice recommended in the last 36 months before policy commencement. It paves the way for honest disclosure during policy applications, further reducing claims processing complications.
#3 Removal of Age Limit
Senior citizens over 65 years of age have difficulty obtaining a comprehensive mediclaim policy. IRDAI has now instructed insurers to provide coverage for everyone regardless of age. This can dramatically increase the number of policyholders in India as more elderly people will come forward to purchase insurance, even with PEDs. Insurers can create customised and innovative products with varying entry age limits. For existing policyholders, it allows for lifetime renewability.
#4 Cashless Claims Approval and Settlement
Insurers are obligated to offer 100% cashless claim settlement without time delay. Requests for cashless authorisation must be answered within one hour of receiving the request, and final authorization for discharge must be approved within three hours. The policyholder should not be made to wait in any case, and any additional charges from the hospital must be paid by the insurer from their shareholder's fund. Digital pre-authorisation can also be issued to expedite this process. In case of death, claim settlement must be done immediately.
#5 Free Look Period and Cancelation
Generally, when you buy a health insurance policy, you are locked for the policy period, which is a year from the date of purchase. IRDAI has allowed a free look period of 30 days, allowing the policyholder to cancel their policy without any charges or penalties. Also, an indemnity-based policy can be cancelled any time during the policy term with 7 days of written notice. The insurer must refund the premium corresponding to the unexpired policy period.
#6 Claims Allowed with Multiple Policies
Individuals may often have different health insurance policies and different providers. They can file a claim settlement with an insurer of their choice as the primary insurer. If the available coverage according to the policy is less than the allowed claim amount, the insurer can get details of other policies and coordinate with other health insurance providers to ensure settlement of the balance amount based on policy conditions. With benefit-based policies, policyholders can claim from all insurers under all policies.
#7 Issuing Customer Information Sheet (CIS)
Every policy provider must provide a standardised CIS containing all the basic policy features explained in simple terms. This increases awareness about health insurance policy and makes it more consumer-friendly. The policyholder can understand coverage, exclusions, and policy benefits with a single look.
Takeaway
IRDAI's measures are meant to standardise insurance operations and improve transparency. It protects policyholders' interests and streamlines claim processing. It can lead to a complete transformation of the insurance industry with more emphasis on user experience, prompting insurers to be more diligent with their services.
Interested in optimal financial protection within your budget? Check out ACKO health insurance plans that are completely customisable to meet your medical insurance needs.
(This article is part of DMCL Consumer Connect Initiative, a paid publication programme. DMCL claims no editorial involvement and assumes no responsibility, liability or claims for any errors or omissions in the content of the article. The DMCL Editorial team is not responsible for this content.)
![submenu-img]() Israel launches strikes on Yemeni Houthi targets after killing dozens of Hezbollah members in Lebanon
Israel launches strikes on Yemeni Houthi targets after killing dozens of Hezbollah members in Lebanon![submenu-img]() Haryana Elections 2024: BJP expels 8 rebels, including Sandeep Garg, for contesting as Independents
Haryana Elections 2024: BJP expels 8 rebels, including Sandeep Garg, for contesting as Independents![submenu-img]() IPL 2025: How much salary will MS Dhoni earn if CSK retain him as uncapped player?
IPL 2025: How much salary will MS Dhoni earn if CSK retain him as uncapped player?![submenu-img]() UPI QR code is down, this is how SBI is fixing the problem
UPI QR code is down, this is how SBI is fixing the problem![submenu-img]() Shocking! Viral influencer who married herself dies by suicide at 26
Shocking! Viral influencer who married herself dies by suicide at 26![submenu-img]() 'पीड़िता का नाम और फोटो नहीं कर सकते उजागर', कोलकाता कांड में सुप्रीम कोर्ट की सख्त टिप्पणी
'पीड़िता का नाम और फोटो नहीं कर सकते उजागर', कोलकाता कांड में सुप्रीम कोर्ट की सख्त टिप्पणी![submenu-img]() MUDA Scam में CM सिद्धारमैया की बढ़ सकती हैं मुश्किलें, ED का कसेगा शिकंजा?
MUDA Scam में CM सिद्धारमैया की बढ़ सकती हैं मुश्किलें, ED का कसेगा शिकंजा?![submenu-img]() Israel Attack On Fateh Sherif: आर-पार के मूड में इजरायल, नसरल्लाह के बाद एक और दुश्मन को किया ढेर
Israel Attack On Fateh Sherif: आर-पार के मूड में इजरायल, नसरल्लाह के बाद एक और दुश्मन को किया ढेर![submenu-img]() Haryana Elections: राहुल गांधी ने हरियाणा में गुटबंदी पर लगाई लगाम, हुड्डा और शैलजा के हाथ मिला दिया बड़ा संदेश
Haryana Elections: राहुल गांधी ने हरियाणा में गुटबंदी पर लगाई लगाम, हुड्डा और शैलजा के हाथ मिला दिया बड़ा संदेश![submenu-img]() 'फीस भरने से चूकने पर अधर में नहीं छोड़ा जा सकता', दलित छात्र के एडमिशन के मामले में SC का बड़ा फैसला
'फीस भरने से चूकने पर अधर में नहीं छोड़ा जा सकता', दलित छात्र के एडमिशन के मामले में SC का बड़ा फैसला![submenu-img]() Mahindra Thar Roxx 4x4 prices revealed, starts at Rs…
Mahindra Thar Roxx 4x4 prices revealed, starts at Rs…![submenu-img]() Sebi gives nod to Hyundai India's Rs 20,000 crore IPO, listing month is...
Sebi gives nod to Hyundai India's Rs 20,000 crore IPO, listing month is...![submenu-img]() Tata launches Nexon iCNG, check price, mileage, other features
Tata launches Nexon iCNG, check price, mileage, other features![submenu-img]() This Indian car brand set to acquire 50% stake in Skoda Auto Volkswagen India, deal will cost Rs…
This Indian car brand set to acquire 50% stake in Skoda Auto Volkswagen India, deal will cost Rs…![submenu-img]() Ford to return to India after 2 years with reopening of....
Ford to return to India after 2 years with reopening of....![submenu-img]() This man was behind IT giant valued at over Rs 13.78 lakh crore, born in Peshawar, also known as father of...
This man was behind IT giant valued at over Rs 13.78 lakh crore, born in Peshawar, also known as father of...![submenu-img]() Meet woman, who scored highest marks in UPSC interview history, not Tina Dabi, Smita Sabharwal, she is...
Meet woman, who scored highest marks in UPSC interview history, not Tina Dabi, Smita Sabharwal, she is...![submenu-img]() Meet India's youngest woman to crack UPSC exam at age 21, secured AIR 13, but didn't become IAS due to...
Meet India's youngest woman to crack UPSC exam at age 21, secured AIR 13, but didn't become IAS due to...![submenu-img]() Meet India’s first female IAS officer, also second woman to crack UPSC exam, she was posted at...
Meet India’s first female IAS officer, also second woman to crack UPSC exam, she was posted at...![submenu-img]() Meet man, bangle seller who cracked UPSC exam despite being specially abled, becomes IAS officer with AIR...
Meet man, bangle seller who cracked UPSC exam despite being specially abled, becomes IAS officer with AIR...![submenu-img]() After Hassan Nasrallah's Death, This Cleric Is Now Tipped To Be Hezbollah Leader | Israel | Lebanon
After Hassan Nasrallah's Death, This Cleric Is Now Tipped To Be Hezbollah Leader | Israel | Lebanon![submenu-img]() Hashem Safieddine, Cousin Of Hassan Nasrallah To Become Hezbollah's New Chief | Israel-Lebanon War
Hashem Safieddine, Cousin Of Hassan Nasrallah To Become Hezbollah's New Chief | Israel-Lebanon War![submenu-img]() Israel Hezbollah War: Nasrallah's Death, A Turning Point for Hezbollah's Future? Experts Explain
Israel Hezbollah War: Nasrallah's Death, A Turning Point for Hezbollah's Future? Experts Explain![submenu-img]() Israel Hezbollah War: Hassan Nasrallah's Death Leads To Protests In J&K, Ex-CM Mehbooba Mufti Reacts
Israel Hezbollah War: Hassan Nasrallah's Death Leads To Protests In J&K, Ex-CM Mehbooba Mufti Reacts![submenu-img]() Israel Hezbollah War: Nasrallah's Death Leads To Protest By Women & Children In Jammu And Kashmir
Israel Hezbollah War: Nasrallah's Death Leads To Protest By Women & Children In Jammu And Kashmir![submenu-img]() Big relief for GST taxpayers: Clear old dues without extra costs; here’s how
Big relief for GST taxpayers: Clear old dues without extra costs; here’s how![submenu-img]() Learn to play the Reliance way, Mukesh Ambani ready to disrupt the toy market
Learn to play the Reliance way, Mukesh Ambani ready to disrupt the toy market![submenu-img]() Ratan Tata's BIG move as Tata Sons set to buy 13% in...
Ratan Tata's BIG move as Tata Sons set to buy 13% in...![submenu-img]() Meet Anuradha who has come out of husband Anand Mahindra's shadow, this is what she does
Meet Anuradha who has come out of husband Anand Mahindra's shadow, this is what she does ![submenu-img]() Mukesh Ambani's BIG gift to shareholders, Reliance earns Rs 53652 crore in just 5 days
Mukesh Ambani's BIG gift to shareholders, Reliance earns Rs 53652 crore in just 5 days![submenu-img]() Haryana Elections 2024: BJP expels 8 rebels, including Sandeep Garg, for contesting as Independents
Haryana Elections 2024: BJP expels 8 rebels, including Sandeep Garg, for contesting as Independents![submenu-img]() Tamil Nadu cabinet rejig: MK Stalin's son Udhayanidhi Stalin is Deputy CM, Senthil Balaji back as minister
Tamil Nadu cabinet rejig: MK Stalin's son Udhayanidhi Stalin is Deputy CM, Senthil Balaji back as minister![submenu-img]() Chandrayaan-3 might have landed in moon's crater, 'ejecta' will reveal secrets
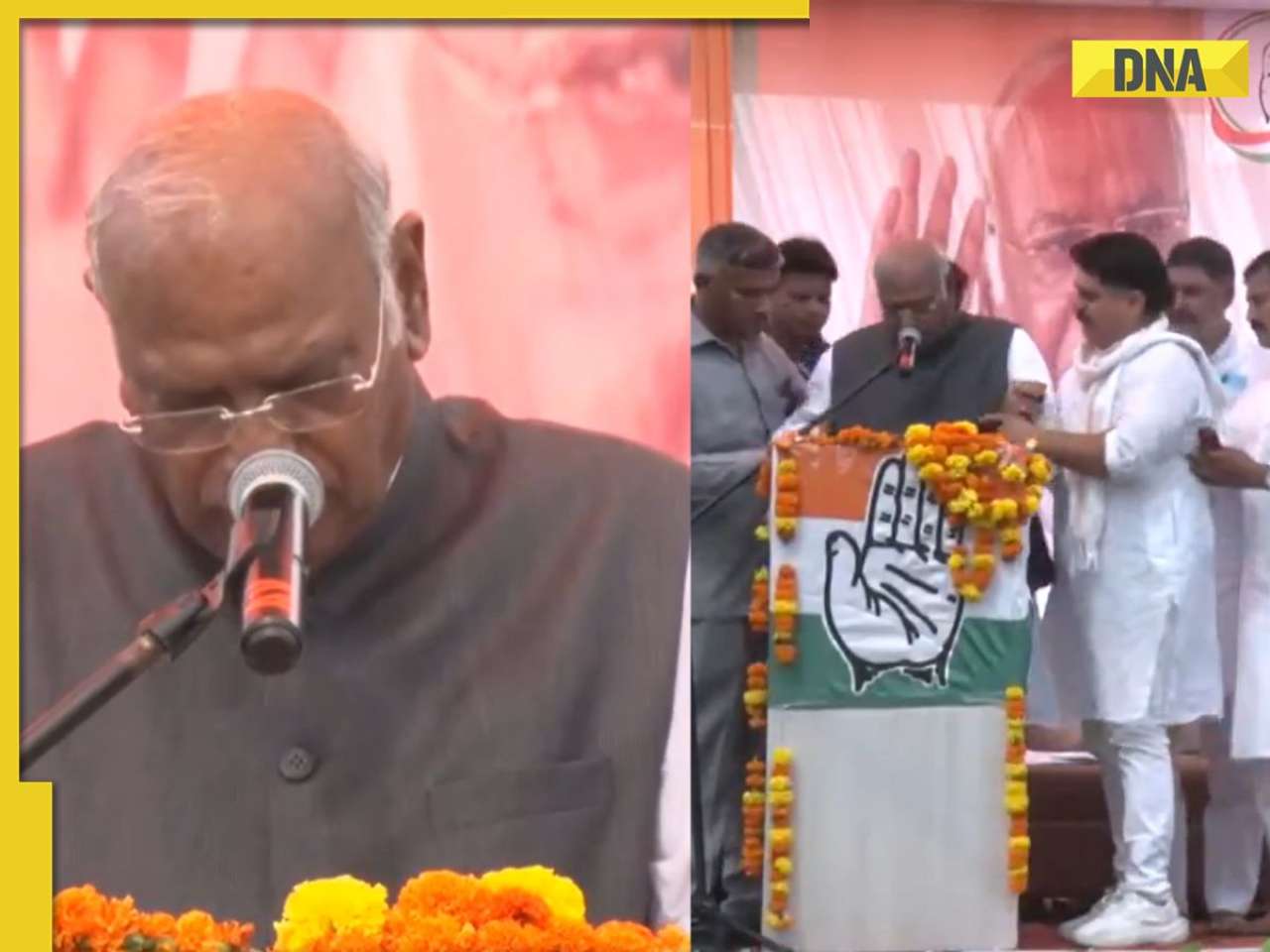
Chandrayaan-3 might have landed in moon's crater, 'ejecta' will reveal secrets![submenu-img]() J-K Elections 2024: Congress chief Mallikarjun Kharge’s health deteriorates during poll rally in Kathua - watch
J-K Elections 2024: Congress chief Mallikarjun Kharge’s health deteriorates during poll rally in Kathua - watch![submenu-img]() Hapur Horror: 5-year-old boy gang raped, assault captured on video, circulated online
Hapur Horror: 5-year-old boy gang raped, assault captured on video, circulated online




































)
)
)
)
)
)
)
)
)
)
)
)
)
)
)




)
)
)
)
)
)